Keeping Smiles Healthy for Children and Young Adults
DentaQuest provides comprehensive dental coverage for Medicaid and CHIP dental members all across Texas.
From Galveston to El Paso, from Dallas to the Rio Grande Valley, we are here to help you understand your child’s benefits so you can make the most of their coverage. No matter where you live, you'll find great dentists and Member support nearby.
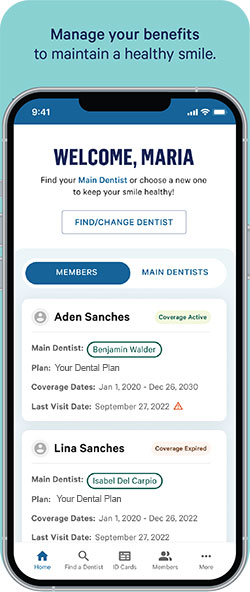
myDentaQuest Mobile App
Make the most of your child’s dental benefits with the myDentaQuest free mobile app for Texas CHIP and Medicaid Members.
Benefits underwritten by DentaQuest USA Insurance Co., Inc.

Oral Health Resources

PREVENTISTRY PULSE
The newsletter designed for anyone who wants to improve oral health for themselves, their families, customers or communities.





