Many in the health care industry hear about integrating medical and behavioral health, but rarely do they discuss the importance of including dental in that paradigm. They forget that the mouth is part of the body, and to be truly healthy, one needs a healthy mouth. After all, oral diseases affect close to four billion people worldwide.
Poor oral health can lead to tooth loss, untreated caries, and periodontal disease, which contribute to adverse health outcomes and high-cost preventable emergency room visits.
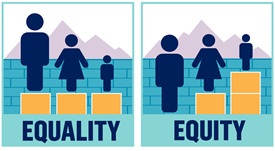
For most people, oral health care in the US is neither easy to obtain nor equitable. With a focus on restorative care and an outdated reimbursement system, dental care delivery in the US is ripe for transformation. Medical-dental integration (MDI) is a key path forward, particularly for vulnerable populations.
What is MDI?
Also called interprofessional practice, MDI is rooted in science that shows addressing health issues holistically—not just oral care at the dental office and physical care at the medical office—improves outcomes and increases access to care.
The separation of medical and dental systems disproportionately burdens vulnerable populations—low-income people, people of color, people with disabilities, rural dwellers, and formerly incarcerated people are all more likely to suffer from dental disease and pain and to report difficulty gaining access to care.
MDI means helping patients get the care they need where they already receive support, creating a system that enables coordination and collaboration among a variety of providers regardless of physical location. It already happens in a number of pilot programs across the country, adding oral health screenings to well-child visits, enabling dental care providers to check insulin levels, using telehealth to connect providers from multiple disciplines with a single patient, and more.
What MDI Can Achieve
Personalized, integrated care plans effectively decrease the number of emergency department visits, reduce overall health care expenditures, and are well received by network providers. MDI can also indirectly drive significant cost saving by addressing undiagnosed systemic disease earlier and enhancing chronic disease management. Yearly savings could reach as high as $100 million if screenings for diabetes, high blood pressure, and high cholesterol occurred during dental care visits, according to the CDC.
To get there, everyone involved in dental care delivery, including software vendors, payers, policymakers, and dental providers, has a role.
- Together we must:
Offer standard, comprehensive dental benefits for any person. - Address the disconnect between public insurance programs where dental benefits may overlap.
- Create a holistic MDI experience for members that will make progress in all four components of the quadruple aim.

PREVENTISTRY PULSE
The newsletter designed for anyone who wants to improve oral health for themselves, their families, customers or communities.